Small & Sick Newborns
Key and Emerging Evidence
This page includes recent research on kangaroo mother care (KMC), recent research on antenatal corticosteroids (ACS), various trials that assessed the efficacy of ACS, and progress reports related to the Every Newborn Action Plan.
Recent Kangaroo Mother Care Global Position and Key Research
Kangaroo mother care: a transformative innovation in health care: global position paper
The purpose of this document is to put forward the joint position and vision of an expert, global, multi-stakeholder working group on implementing KMC for all preterm or LBW infants as the foundation for small and/or sick newborn care within maternal, newborn and child health programs, and spur collaborative global action. Reversing the long-standing inequities in health care will require prolonged efforts; the scale-up of KMC as an essential service for all mothers and their preterm or LBW infants as a critical component of universal health coverage can serve as the key starting point.
Highlights
- Kangaroo mother care (KMC) is an intervention that enables the mother to take a central role in her own and her newborn’s care, thereby ensuring the power stays with the mother, and health workers support and respond to the mother’s and newborn’s needs.
- It humanizes maternal and newborn care by empowering and involving those who care most for the infant, rather than focusing predominantly on technological solutions.
- KMC can serve as a starting point for broader health-system redesign and service delivery transformation for maternal and newborn care, and a model of what can be accomplished when relevant stakeholders are empowered to play the roles naturally entrusted to them in the care of their newborns.
Operationalizing this concept can serve as a strong foundation of highly efficient health systems that are rooted in the communities they serve and focus not only on preventing and treating illness but also on improving well-being and quality of life.
Kangaroo mother care, or KMC, a type of newborn care involving skin-to-skin contact with the mother or other caregiver and exclusive breastfeeding, reduces mortality in infants with low birth weight (<2.0 kg). KMC is often initiated after the newborn has been stabilized. However, the majority of newborn deaths occur before stabilization. The results of a new clinical trial published in May 2021 in the New England Journal of Medicine, provide evidence in support of starting KMC immediately after birth, a clear message that keeping mothers and babies together helps babies to survive and thrive.
Key Findings
- Starting KMC immediately after birth in newborns with birthweight of 1000 grams to 1799 grams has the potential to save up to 150,000 more lives each year (a further increase in survival of 25%), compared with the current recommendation of starting it only once a baby is stable.
- Mother-Newborn Intensive Care Units will be critical to support the mother, or a surrogate, in providing this immediate, ongoing skin-to-skin contact from birth.
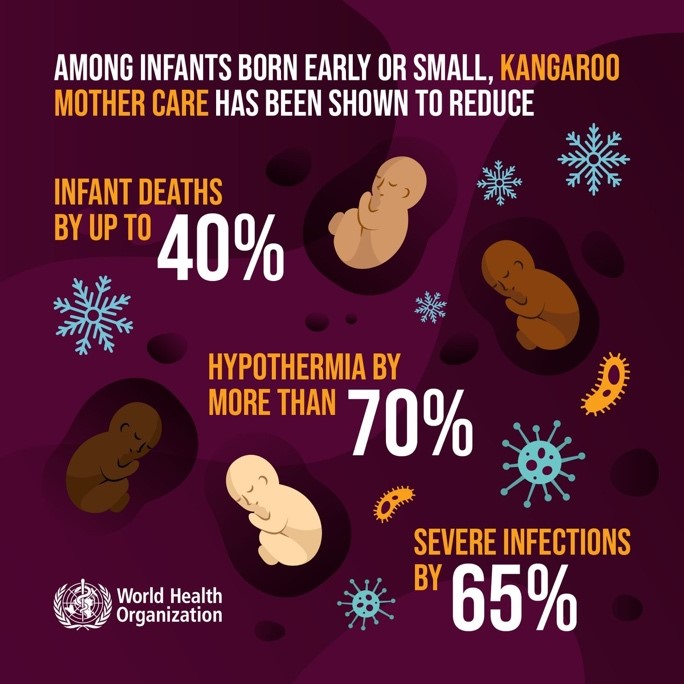
Understanding of the lifesaving benefits of KMC for babies born early or small and its continued importance during the COVID-19 pandemic are further strengthened with this new evidence on the benefits of starting the intervention immediately after birth. Among preterm or low birthweight infants, KMC has been shown to reduce infant deaths by as much as 40%, hypothermia by more than 70%, and severe infections by 65% (see figure below). As the authors write in a recent AlignMNH blog post. “The study has the potential to bring about a paradigm shift in how small and sick newborns are cared for immediately after birth, laying the path for zero separation of LBW babies from their mothers.” This new evidence was also discussed in a recent webinar supported by WHO’s Quality of Care Network, with continued conversation with the webinar panelists here.
Recent Research on Antenatal Corticosteroids
The use of antenatal corticosteroids (ACS) for pregnant women at risk of preterm delivery has proved to be one of the most effective hospital-based interventions to reduce neonatal mortality associated with preterm birth. The 2015 ACT trial aimed to access the feasibility, effectiveness, and safety of a multifaceted intervention designed to increase the use of ACS in six low-and middle-income countries. Findings indicated that despite the use in low-birthweight infants, neonatal mortality did not decrease in intervention groups and could lead to other harm, including increased maternal infection. An important point of discussion was limitations of the study, including the use of birthweight percentile instead of gestational age, which could determine a woman’s eligibility to safely receive ACS. Because of these findings, the WHO recommended in 2015 that ACS should be used for women at risk of preterm birth from 24 to 34 weeks of gestation when the following conditions are met:
- Gestational age assessment is accurately undertaken
- Preterm birth is considered imminent
- There is no evidence of maternal infection
- Adequate childbirth care is available (including the capacity to recognize and safely manage preterm labor and birth)
- The preterm newborn can receive adequate care if needed (including resuscitation, thermal care, feeding support, infection treatment, and safe oxygen use)
The WHO ACTION-I (Antenatal Corticosteroids for Improving Outcomes in Preterm Newborns) trial was randomized trial to assess the safety and efficacy of dexamethasone (an ACS) in women in hospitals in low-resource countries who were at risk for early preterm birth. However, it’s important to note that the study invested resources in careful selection of appropriate clients and settings for the intervention, as well as a range of interventions, capacity building, and other factors to support a higher level of care for women and newborns at study sites.
A Cochrane review analysis (of 27 randomized trials including 11,272 women and 11,925 neonates) assessed the effect of administering a course of corticosteroids to women prior to anticipated preterm birth (before 37 weeks) on fetal and neonatal morbidity and mortality, maternal morbidity and mortality, and childhood development later in life. Evidence supports the continued use of a single course of ACS to accelerate fetal lung maturation in women at risk of preterm birth to reduce the risk of serious respiratory illness and death in neonates in low- and middle-income countries.
Neonatal outcomes from this analysis found:
- Reduced risk of perinatal death (numbers of stillbirths and babies dying in the first 28 days of life)
- Reduced risk of early neonatal death (numbers of babies dying in the first 28 days of life)
- Reduced risk of severe respiratory distress at 24 hours after birth
- Minor effect on babies’ birth weight
Other Resources on ACS:
Frequently Asked Questions (FAQs) Regarding Antenatal Corticosteroids for Fetal Maturation
UN Commission/Born Too Soon Care Group on Antenatal Corticosteroids, 2013
This brief has answers to some of the most frequently asked questions regarding antenatal corticosteroids including the use, effectiveness, and special circumstances responses.
Born Too Soon: The Global Action Report on Preterm Birth
March of Dimes, PMNCH, Save the Children, WHO, 2012
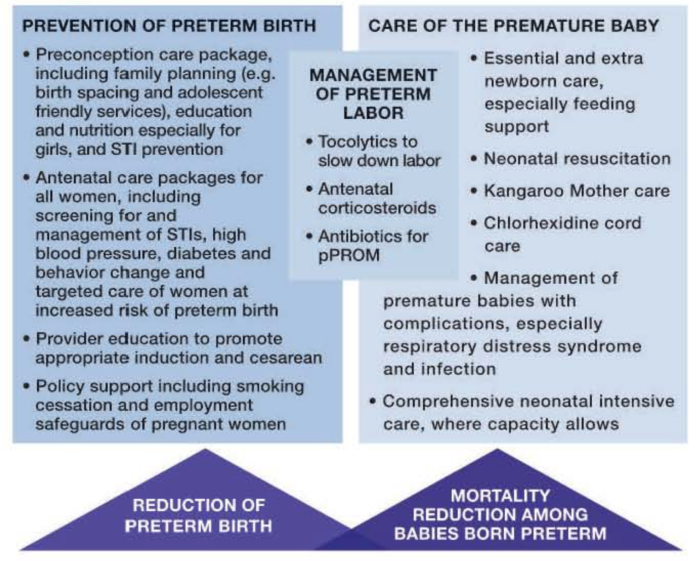
Published in January 2016, this Lancet series on ending preventable stillbirths remains a critical global resource in highlighting missed opportunities to This report was a foundational exploration into the global burden of prematurity and helped establish it as a global maternal and newborn health (MNH) priority. It includes the first-ever preterm birth rates by country and authored by 45 multi-disciplinary experts from 11 countries, with almost 50 organizations in support. The report provides an analysis on the incidence and prevalence of preterm birth, as well as evidence-based interventions to prevent preterm birth and reduce deaths among premature babies, see figure below.