Time for a Big Stride Forward in Maternal and Newborn Health
Only two decades ago, for every 1,000 live births, about 3.4 women and 52 babies died late in pregnancy or during the neonatal period. We have since witnessed an impressive decline in maternal and newborn mortality to an estimated 2.1 women and 31 late fetal and newborn deaths. And because fertility also declined, the number of deaths declined even more. But we are still far from the Sustainable Development Goals (SDGs) of 0.7 maternal deaths and 12 neonatal deaths per 1,000 live births, as well as global targets of 12 or fewer stillbirths per 1,000 total births by 2030. Are we ready for a big stride forward?
AlignMNH focuses on priority issues for mothers and newborns and prevention of stillbirths. Nearly half of all maternal deaths and 40% of all stillbirths and neonatal deaths occur during labor and on the day of birth. Surely, as societies, we can guarantee 48 hours of quality care to welcome each newborn into the world. This means every woman and every baby must receive high-quality routine delivery care and, if necessary, emergency care in the same facility or at a facility within timely reach.
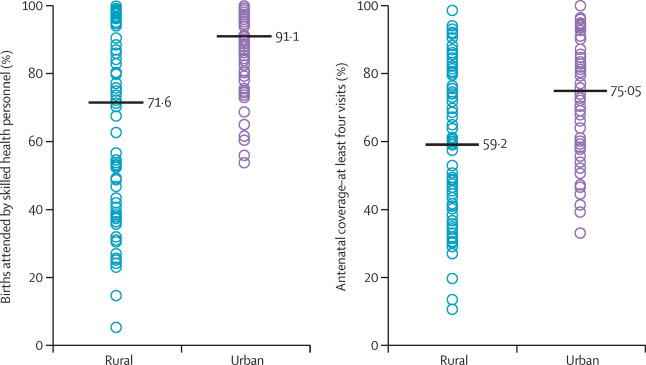
Health facility delivery and skilled birth attendant coverage are finally increasing almost everywhere, and fast. Although delayed the longest among all basic interventions, facility deliveries and skilled birth attendance in many countries accelerated after the year 2000, according to national surveys.
These trends are no guarantee of good quality care, however, and have not yet yielded the expected survival results. Health workers’ lack of skills and poor practices and health facility capacity are major impediments in many countries, which struggle with inadequate training and supervision programs and erratic supply chains. But there are also structural causes, such as shortages of capable nurses and midwives, especially in rural settings, an increase in the number of deliveries in small, under-equipped facilities, and low quality of services for poor women in urban settings.
Data, especially from household surveys, play an instrumental role in driving progress in maternal and newborn health. With less than 10 years remaining to reach the SDGs, now is the time for a reset in what data are collected. Fortunately, we have better evidence to guide a data-driven all-out effort to further reduce maternal and newborn mortality and prevent stillbirths.
The longer-term goal is for all countries to have a fully functional birth and death registration system that includes stillbirths and causes of death. In the meantime, sample registration systems should be established to fill the mortality and causes of death data gaps. Special efforts are required for maternal and newborn mortality and stillbirths, as under-registration is often the rule rather than the exception.
Second, we now know that household surveys can be more detailed by using full pregnancy histories to collect data on late fetal and newborn mortality at little extra cost. Collecting maternal mortality data in sibling survival histories remains an imperfect method: long reference periods, large confidence intervals and no disaggregation.
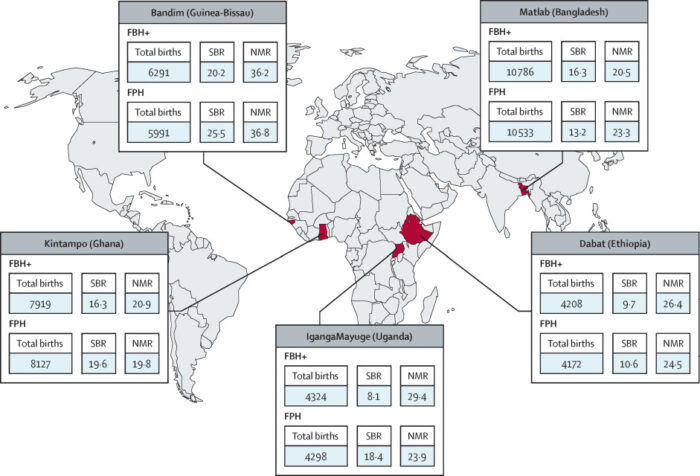
Third, use of routine health facility data is critical to obtain better local and real-time information about quality of care. A recent five-country study showed us the way. The quality of the hospital maternity registers was good enough to obtain several indicators, with potential to expand and enhance. COVID-19 has generated a new wave of interest in routine health facility data to document the pandemic’s impact on continuation of essential health services. This should lead to greater future investments, particularly if data are made more accessible.
Fourth, counting and auditing every health facility death is essential for effective action and accountability. Maternal death surveillance and response systems need a major boost to overcome common implementation challenges. Perinatal deaths can be included, as shown in high-income countries, but probably best in a well-supported sample of health facilities to ensure good data quality.
Fifth, digital longitudinal registers that follow individual pregnant women and their babies until at least 6 weeks after delivery are within reach. The Global Network and the AMANHI multicountry studies illustrated the wealth of data and insights gained from such an approach. The rollout of such registers, including data access for analysts, is taking much longer than anticipated but now is the time to scale up.
Lastly, facility surveys are needed to monitor service coverage, service quality and data quality on a regular basis. Here, too, the COVID-19 pandemic may provide impetus, with countries starting to use regular phone or web-based surveys to monitor health facility services and other indicators.
The time is ripe for a renewed major stride forward in maternal and newborn health and survival, grounded in an evidence-based approach for local action and accountability.
Ties Boerma, University of Manitoba; Oona Campbell, London School of Hygiene and Tropical Medicine; and Agbessi Amouzou, Johns Hopkins University as part of the Countdown to 2030 for Women’s, Children’s & Adolescents’ Health