Provision of Care
Global recommendations and guidance
Recent WHO guidance on provision of high quality MNH care across the continuum of care, outlines best clinical practices and incorporates the principles of experience of care and respectful care:

- 2016 WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience: This comprehensive WHO guideline provides global, evidence-informed recommendations on routine antenatal care (ANC). This guideline covers recommendations in various areas including nutrition, maternal and fetal assessment, preventative measures, interventions for common physiological symptoms and interventions to improve ANC utilization and quality of care.

- 2017 Second Edition of WHO’s Managing Complications in Pregnancy and Childbirth (MCPC): Since 2000, this manual has been used globally to guide the care of women and newborns who have complications during pregnancy, childbirth and the immediate postnatal period. The MCPC manual targets midwives and doctors working in district-level hospitals. Updates throughout the 2017 second edition MCPC reflect the importance of respectful care for mothers and newborns. Several updated chapters on symptoms refer the reader to a set of basic principles when providing care, reinforcing the importance of respectful care as a key element of quality care. WHO, with the MCSP project, also prepared a related brief.

- 2018 WHO Recommendations: Intrapartum Care for a Positive Childbirth Experience: This up-to-date, comprehensive and consolidated 2018 guideline on essential intrapartum care brings together new and existing WHO recommendations that, when delivered as a package, will ensure good-quality and evidence-based care irrespective of the setting or level of health care. The recommendations in this guideline are intended to inform the development of relevant national- and local-level health policies and clinical protocols.
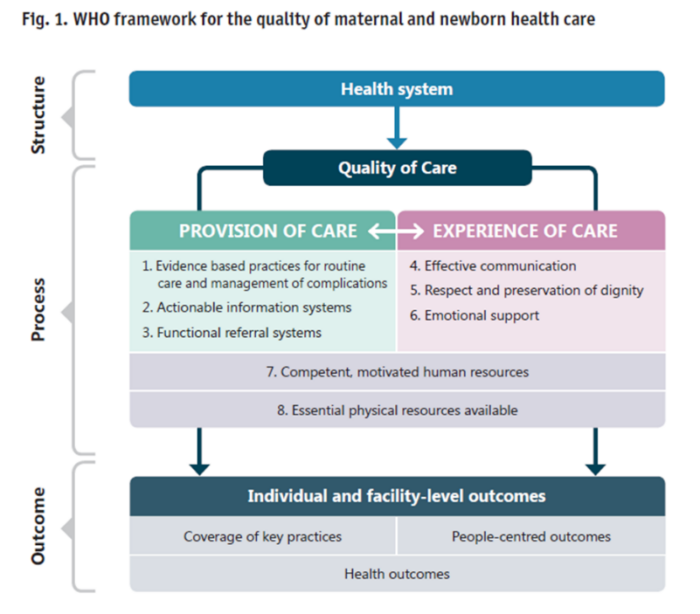
In 2015, WHO published a vision for MNH that includes eight quality domains related to provision of care, experience of care and cross-cutting health system functions (see Fig. 1). In 2016, WHO published Standards for improving quality of maternal and newborn care in health facilities. This framework for improving the quality of care for mothers and newborns around the time of childbirth encompasses both the provision and experience of care and key health system functions necessary to achieve quality health care. The framework contains eight aspirational domains of quality of care and associated actionable quality statements that should be assessed, improved and monitored within the context of the health system building blocks
Issued by WHO in 2020, Standards for improving quality of care for small and sick newborns in health facilities define eight aspirational standards and associated actionable quality statements for improving quality of inpatient care for small and sick newborns, building on essential newborn care and ensuring consistency with the WHO quality of care framework. This is a resource for policy-makers, health care professionals, health service planners, program managers, regulators, professional bodies and technical partners.
In 2017, WHO and partners launched a multi-country Network to improve quality of maternal newborn and child health care – The Network for Improving Quality of Facility-based Maternal, Newborn and Child Care. The Network website includes many useful resources, including implementation guidance focused on key policy, governance structures and actions at national, subnational and facility level and a QoC MNCH Network Monitoring Framework with priority QoC indicators for use by national/subnational managers and facility managers and health workers. The Monitoring framework includes an appendix of recommended common MNH quality of care indicators (Appendix 1) and a ‘catalogue’ of flexible MNH QoC indicators categorized by Quality Statement for use by QI teams working to improve care in specific technical area.
In the 2021 report, Survive and thrive: transforming care for every small and sick newborn, WHO maps a pathway towards 2030 to achieve the SDG target to end preventable newborn deaths. The report outlines the global problem, showcases progress, summarizes what can be done to transform inpatient care for small and sick newborns, and demonstrates the importance of data to guide investment and improve quality of care and equity. The report builds on the Every newborn: an action plan to end preventable deaths. Strategic objective two, improve the quality of maternal and newborn care, emphasizes that quality of care is not only essential to newborn survival, but it imperative to newborns thriving. It also stresses the importance of a hospital environment that actively welcomes and engages parents in the care of their newborn, along with promoting quality-improvement to advance provider skills and competencies.
The 2021 Nurturing Care Thematic Brief from WHO outlines the importance of nurturing care and its five interrelated components, as well as examples and practical actions to strengthen nurturing environments for newborns, including those who are born too soon, small or sick. It also includes six case studies that illustrate what can be done to create a nurturing environment and enable caregivers to provide nurturing care for their newborns beginning at a health facility and continuing at home.
- Good health: Preventing and managing illness, including evidence based-high quality care for small and sick newborns
- Adequate nutrition: Optimizing exclusive breastfeeding or breast milk feeding, including for small and sick newborns
- Safety and security: Warmth, good hygiene, minimizing stress, and enabling the primary caregiver, most commonly the mother, to be with the infant in a quiet environment
- Early learning: Stimulating the baby’s brain through touch, voice, or contact
- Responsive caregiving: Being aware of the newborns’ signals, which may indicate readiness to feed, pain or stress, and responding to them appropriately.
