Maternal and newborn health are inextricably connected. Each year, 295,000 women die due to pregnancy-related causes; more than 2 million babies are stillborn, half during labor; and 2.5 million newborns die within the first month of life. 99% of these maternal and newborn deaths occur in low- and middle-income countries, and disproportionally within the poorest families; most of these deaths are preventable. [1] [2] [3] Addressing the health needs of women during pregnancy, labor and birth, and postpartum period together with those of their newborns – to integrate planning, services, and strategies about maternal health with those about newborn health – makes intuitive sense.
Emphasizing the mother-baby dyad offers a practical approach: Women and families are more satisfied with coordinated, combined care; and the same provider is often responsible for both preventative and life-saving interventions that protect both women and their newborns. Integrated approaches increase efficiency and lower costs. Most importantly, focusing on the mother-baby dyad, on that central relationship between a woman and her newborn, helps both of them survive. [4]
Causes of death and other poor outcomes are interconnected for pregnant women and their babies, and the critical periods of care for both women and newborns (primarily, at the time of birth) overlap. For instance, complications in labor may cause maternal, fetal, or newborn death and long term disabilities. [5] Collaboration along the continuum of care is necessary to realize our goals for maternal and newborn deaths and preventing stillbirths.
The leading causes of maternal death are direct causes which account for nearly 75% of maternal deaths:
- Hemorrhage (27.1%) – mostly postpartum hemorrhage (PPH)
- Hypertensive disorders (14%), e.g., pre-eclampsia/eclampsia
- Sepsis (10.7%) – usually following births
Indirect causes, such as HIV-related causes or medical disorders, account for approximately 25% of deaths. [6]
75% of all newborn deaths result from three preventable and treatable conditions:
- Complications due to prematurity,
- Intrapartum-related events (including birth asphyxia), and
- Neonatal infections.
While 2.6 million stillbirths occur each year. [7]
This concept articulates critical linkages in time (when care is given along the lifecycle) and place (where, or at what level of the health system, care is delivered), to move towards greater coverage of critical, evidence-based interventions. When women and newborns receive high quality care during pregnancy, at the time of birth, and in the early postnatal period, women stay healthy and babies get the best start in life.
In other words, supporting integrated packages of essential, proven interventions for women and newborns – delivered by a skilled attendant at a time and place that is feasible and acceptable – saves lives.
Featured Topics
Focusing on mother-baby dyad helps both survive
Major causes of maternal and newborn morbidity and mortality are linked
The maternal, newborn, and child health continuum of care concept naturally supports an integrated MNH approach, with the mother-baby dyad at the center

Emphasizing the mother-baby dyad offers a practical approach: Women and families are more satisfied with coordinated, combined care; and the same provider is often responsible for both preventative and life-saving interventions that protect both women and their newborns. Integrated approaches increase efficiency and lower costs. Most importantly, focusing on the mother-baby dyad, on that central relationship between a woman and her newborn, helps both of them survive. [4]
NEW WHO Recommendations on Maternal and Newborn Care for a Positive Postnatal Experience
On March 30, 2022, the World Health Organization released guidance on maternal and newborn care for a positive postnatal experience. A total of 63 recommendations on maternal care, newborn care, health systems, and health promotion address individual patient care and service delivery. The executive summary is available in Arabic, Chinese, English, French, Portuguese, Russian, and Spanish.
The new guidelines respond to global trends in maternal-newborn morbidity and mortality. As death rates drop globally, the new guidelines place great emphasis on thinking beyond survival, and continue to provide guidance on essential interventions to continue reductions in maternal and newborn mortality. Here is what’s new:
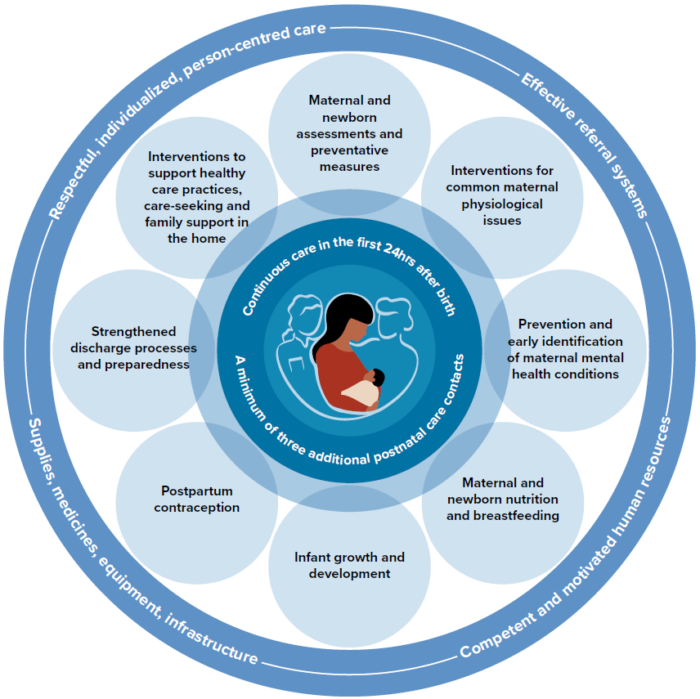
- The importance of family-centered care | The new guidelines address the importance of the home and whole family in the health of the mother-baby dyad, including specific guidelines for the inclusion of men in care plans, the use of home-based medical records, and assessment of the home environment prior to discharge.
- Increased focus on maternal well-being | Moving beyond survival for the mother, the new guidelines address maternal mental health and comfort, including specific guidelines for pain control following delivery, and universal screening and intervention for depression and anxiety.
- Thinking beyond survival for the newborn | Interventions during the hours, days, and weeks following birth can have long-lasting impact on the health and well-being of children. The new guidelines specifically address responsive care, early infant development, safe sleep, and screening for hearing and eye abnormalities.
- Tackling health system and workforce challenges | The new guidelines recommend several strategies for increasing the size and quality of the healthcare workforce needed for a positive postnatal experience, including specific recommendations about mobilizing a greater diversity of health workers, establishing midwife-led continuity of care models, and using digital tools to improve birth registration and health behaviors in the home. The new guidelines also recommend integration of complementary maternal-newborn services when possible (maternal mental health and early infant development) and routine screening and prevention of infectious diseases (de-worming, TB, HIV screening).
Scaling Essential Interventions Can Save 3 Million Lives Each Year
By scaling up essential interventions, around 3 million lives can be saved every year (see Fig. 1), approximately half in Africa. The greatest impact for the mother-baby dyad along the continuum of care is providing quality care during labor and childbirth, and care of the small and sick newborn. Yet, these interventions have the lowest coverage and highest equity gap.
Figure 1.
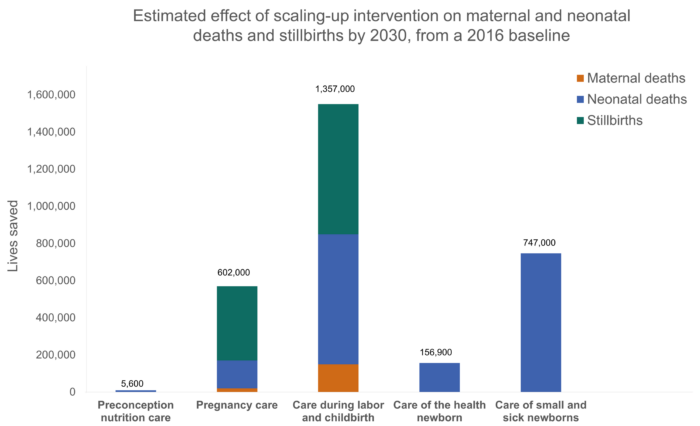
Aligning collective action around the mother-baby dyad globally is needed to accelerate gains for women, newborns, families, and communities. Read more on our Blog: Embarking on a Decade of Action to Promote the Mother-Baby Dyad
Key Messages from the World Health Organization’s 2021 Four Updated Recommendation on the Prevention and Treatment of Maternal Peripartum Infections
- Bacterial infections around the time of childbirth account for about one-tenth of maternal deaths and contribute to severe morbidity and long-term disability for many affected women.
- For antibiotic prophylaxis for caesarean section, WHO recommends a single dose of first-generation cephalosporin or penicillin in preference to other classes of antibiotics, given 30–60 minutes prior to skin incision.
- WHO recommends vaginal preparation with povidone-iodine (1% to 10%) or chlorhexidine gluconate (0.05% to 0.25%) for 30 seconds immediately before caesarean section in all women undergoing caesarean section.
- For preoperative skin preparation for caesarean section, WHO recommends use of alcohol-based chlorhexidine gluconate (e.g., 2% chlorhexidine gluconate in 70% alcohol) in preference to other antiseptic agents; where chlorhexidine gluconate is not available, other antiseptic agents such as povidone-iodine can be considered a suitable antiseptic agent for preoperative skin preparation, although it is not as effective as alcohol-based chlorhexidine gluconate.
- WHO recommends routine antibiotic prophylaxis for women undergoing operative vaginal birth (i.e., vacuum assisted vaginal delivery or forceps; available evidence, from high-income countries, strongly supports the use of a single dose of intravenous amoxicillin (1 g) and clavulanic acid (200 mg) administered as soon as possible after birth and no more than 6 hours after birth; where this combination is not available, provider should consider the use of an alternative regimen based on similar spectrum of activity, safety profile, availability and cost.
Four Updated WHO Recommendations on the Prevention and Treatment of Maternal Peripartum Infections
Recommendation: For antibiotic prophylaxis for caesarean section, a single dose of first-generation cephalosporin or penicillin should be used in preference to other classes of antibiotics.
Summary of clarifying remarks:
- For antibiotic prophylaxis for caesarean section, a single dose of first-generation cephalosporin or penicillin should be used in preference to other classes of antibiotics. This antibiotic choice is based on 1) effectiveness, and 2) as part of efforts to contain antimicrobial resistance.
- However, the choice of an antibiotic should be adapted to the local context: informed by local antimicrobial resistance guidance, local bacteriologic patterns of post-caesarean infectious morbidity, safety profile, the clinician’s experience with that particular class of antibiotics, availability and cost.
- Prophylactic antibiotics are recommended for women undergoing elective or emergency caesarean section and should be given 30–60 minutes prior to skin incision, rather than intraoperatively after umbilical cord clamping.
- Emphasizes the importance of using a simple and short (single dose, 30–60 minutes before surgery) antibiotic regimen for prophylaxis, unless there are other clinical factors for consideration (e.g. high maternal body mass index, prolonged labour, prolonged duration of surgery, extensive surgical manipulation or massive blood loss) that might increase the risk of developing post-caesarean infections. Clinical judgement is needed to evaluate if a different regimen (e.g., higher dose, second dose) of prophylactic antibiotics is warranted in the presence of risk factors.
Summary of clarifying remarks:
- All women undergoing caesarean section should have vaginal cleansing with povidone-iodine (1% – 10%), for 30 seconds performed immediately before caesarean section (e.g. directly following preoperative urinary bladder catheterization to minimize the woman’s discomfort).
- While the evidence on vaginal preparation before caesarean section was largely derived from trials using povidone-iodine, benefit was demonstrated overall for any antiseptic (either povidone-iodine or chlorhexidine gluconate) versus no antiseptic. Included trials used varying concentrations of chlorhexidine gluconate (0.05% to 0.25%) or povidone-iodine (1% to 10%), and the base (aqueous or alcohol) was not described. Alcohol-based antiseptic solutions should not be used for vaginal preparation because of concerns around irritation of mucosa.
- This recommendation pertains to all women undergoing caesarean section regardless of their baseline risk of infectious morbidity following surgery (i.e. for caesarean section in women before or during labour, and women with intact or ruptured membranes).
- Vaginal preparation should be performed as close to the start of caesarean section as possible (e.g. directly following preoperative urinary bladder catheterization) to minimize the woman’s discomfort.
- The duration of vaginal preparation varied from 30 seconds to one minute. The Guideline Development Group noted that shorter application, i.e., 30 seconds, and contact time are likely to be associated with less maternal and fetal exposure, which is desirable.
Recommendation a: The use of alcohol-based chlorhexidine gluconate for skin preparation prior to elective or emergency caesarean section is recommended.
Recommendation b: The method of application of alcohol-based chlorhexidine gluconate prior to caesarean section should be based primarily on instructions for use, the clinician’s experience and preferences.
Summary of clarifying remarks:
- There was a lack of evidence to recommend a specific concentration of chlorhexidine gluconate; however, most trials included used 2% chlorhexidine gluconate in 70% alcohol.
- Where chlorhexidine gluconate is not available, other antiseptic agent such as povidone-iodine can be considered a suitable antiseptic agent for preoperative skin preparation, although it is not as effective as alcohol-based chlorhexidine gluconate.
- A standard preoperative skin preparation technique that is appropriate for the intended skin incision must be followed (e.g., allow antiseptic agent to dry and not wiping off).
Recommendation: Routine antibiotic prophylaxis is recommended for women undergoing operative vaginal birth.
Summary of clarifying remarks:
- “Operative vaginal birth” is the term used to describe delivery of the fetal head assisted by either vacuum extractor or forceps.
- Available evidence, from high-income countries, strongly supports the use of a single dose of intravenous amoxicillin (1 g) and clavulanic acid (200 mg) administered as soon as possible after birth and no more than 6 hours after birth.
- Intravenous amoxicillin and clavulanic acid may not be readily available or feasible to use in resource-limited settings and suggested that where this combination is not available, providers should consider the use of an appropriate class of antibiotics with similar spectrum of activity, based on local antimicrobial resistance patterns, safety profile (including allergies), the clinician’s experience with that class of antibiotics, availability and cost.
- This recommendation relates to the use of antibiotics for women who are undergoing operative vaginal birth and who are not receiving postpartum antibiotics for other indications.
Highlighted Resources Across the Continuum of Care
AlignMNH has curated an initial set of resources related to the mother-baby dyad and the phases shared by mothers and babies (pregnancy, childbirth, postnatal period). We will continuously update and add to these resources.
This article presents an updated series of cause-specific mortality for neonates and children younger than 5 years from 2000 to 2019. In 2019, there were 5·30 million deaths (95% uncertainty range 4·92–5·68) among children younger than 5 years, primarily due to preterm birth complications (17·7%, 16·1–19·5), lower respiratory infections (13·9%, 12·0–15·1), intrapartum-related events (11·6%, 10·6–12·5), and diarrhoea (9·1%, 7·9–9·9), with 49·2% (47·3–51·9) due to infectious causes.
Trends in Maternal Mortality: 2000 – 2017, WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division, 2019
This report provides global, regional, and country-level estimates and trends for maternal mortality covering the period of 2000-2017. The report notes that the SDG goal to end preventable maternal deaths by 2030 will not be achievable given the current rate of reducing maternal deaths.
A Neglected Tragedy: The Global Burden of Stillbirths, UN Inter-agency Group for Child Mortality Estimation, 2020
This report highlights the slow progress in reducing stillbirth rates compared to other maternal and newborn health outcomes. The report calls out a need for better measurement and data of stillbirths as well as improved quality of care during pregnancy and birth.
Every Child Alive, The Urgent Need to End Newborn Death, UNICEF, 2018
This 2018 report from UNICEF outlines the global challenge of keeping every newborn alive, presents data on where newborns deaths are occuring, proposes an agenda for action that addresses both expanding access and improving quality of care, and offers a way forward that focuses on place (clean, functional health facilities), people (well trained health workers), products (life-saving drugs and equipment), and power (dignity, respect, and accountability).
Undernourished and Overlooked: A Global Nutrition Crisis in Adolescent Girls and Women, UNICEF, 2023
Undernutrition, micronutrient deficiencies and anemia amplify gender inequalities by lowering learning potential, wages and life opportunities for adolescent girls and women, weakening their immunity to infections, and increasing their risk of life-threatening complications during pregnancy and childbirth. The report findings reveal a lack of progress on nutrition in adolescent girls and women in the last two decades and that the global food and nutrition crisis is now pushing millions of mothers and their young children in to malnutrition and hunger. Without urgent action from governments and the international community, the consequences could last for generations to come.
In November 2021, a Scoping review of interventions to maintain essential services for maternal, newborn, child and adolescent health and older people during disruptive events was published by the World Health Organization (WHO) Department of Maternal, Newborn, Child and Adolescent Health and Ageing. This review of published and grey literature aims to identify interventions implemented to maintain the provision and use of essential services for MNCAH during disruptive events and to summarize lessons learned during these interventions.
WHO Recommendations on Antenatal Care For a Positive Pregnancy Experience, WHO, 2021
This comprehensive WHO guideline (2016) provides global, evidence-informed recommendations on routine antenatal care. This guideline covers recommendations in various areas including nutrition, maternal and fetal assessment, preventative measures, interventions for common physiological symptoms and interventions to improve antenatal care utilization and quality of care. Additional resources on antenatal care can be found on the WHO website here.
WHO Recommendations: Intrapartum Care for a Positive Childbirth Experience, WHO, 2018
This up-to-date, comprehensive and consolidated 2018 guideline on essential intrapartum care brings together new and existing WHO recommendations that, when delivered as a package, will ensure good-quality and evidence-based care irrespective of the setting or level of health care. The recommendations in this guideline are intended to inform the development of relevant national- and local-level health policies and clinical protocols.
More than a third of maternal deaths and a substantial proportion of pregnancy-related, life-threatening conditions are due to complications that arise during labor, childbirth, or the immediate postpartum period. Improving quality of care around the time of birth is essential for reducing stillbirths and maternal and newborn deaths. This technical brief from MOMENTUM Country and Global Leadership reviews 26 new recommendations from the WHO’s 2018 recommendations on intrapartum care for a positive childbirth experience, and recommends policy and program considerations for countries adopting, adapting, and implementing the recommendations.
Key messages:
- The World Health Organization guideline recognizes a “positive childbirth experience” as a significant goal for all women while in labour and while giving birth.
- The recommendations aim to:
- Promote “normality”
- Reduce variation in care
- Promote nonclinical intrapartum practices that optimize quality of care and improve women’s comfort, maternal and perinatal outcomes, and experience of care
- Highlight unnecessary, non-evidence-based, and potentially harmful intrapartum care practices
WHO Labour Care Guide, WHO, 2020
This 2020 manual has been developed to help skilled health personnel to successfully use the WHO Labour Care Guide. The WHO Labour Care Guide is a tool that aims to support good-quality, evidence-based, respectful care during labour and childbirth, irrespective of the setting or level of health care.
An article published in August 2019 in BMJ Global Health describes an innovative, dynamic approach that is being used by WHO to respond to new, important evidence in the area of maternal and perinatal health. This new approach, called “living guidelines”, uses a combination of continuous literature surveillance, rapid updating of prioritized systematic reviews and virtual consultations with “living guideline” panels to update and develop new WHO recommendations. This can ensure that the latest evidence and updated recommendations can reach health workers worldwide as quickly as possible.
WHO Recommendations on Interventions to Improve Preterm Birth Outcomes, WHO, 2015
Issued by WHO in 2015, this document offer policy makers and program managers guidance for developing job aids and tools in pre or in-service training to strengthen delivery of MNH care related to preterm birth.
WHO Standards for improving quality of maternal and newborn care in health facilities, WHO, 2016
This framework for improving the quality of care for mothers and newborns around the time of childbirth, developed by WHO and released in 2016, encompasses both the provision and experience of care. It contains eight domains of quality of care that should be assessed, improved and monitored within the context of the health system building blocks.
WHO Standards for improving the quality of care for small and sick newborns in health facilities, WHO, 2020
Issued by WHO in 2020, these standards for the care of small and sick newborns in health facilities define, standardize and mainstream inpatient care of small and sick newborns, building on essential newborn care and ensuring consistency with the WHO quality of care framework. A resource for policy-makers, health care professionals, health service planners, program managers, regulators, professional bodies and technical partners.
Accelerating Improvements in Breastfeeding at Scale: Insights from Bangladesh, Alive & Thrive and AlignMNH, 2021
Since its inception in 2009, Alive & Thrive, has focused on increasing early initiation, exclusive and continued breastfeeding as part of its efforts to strengthen maternal, newborn, and child health and wellness. Alive & Thrive partners with national and sub-national stakeholders at various levels to strengthen breastfeeding awareness and support within health systems and policy environments, and to introduce and scale up data-driven social behavior change approaches that address breastfeeding barriers. In this brief, we discuss the benefits of breastfeeding, global breastfeeding recommendations, and key takeaways on Alive & Thrive’s implementation experience in Bangladesh.
The Role of Midwives and Nurses in Protecting, Promoting, and Supporting Breastfeeding, UNICEF, World Health Organization, Global Breastfeeding Collective
Midwives and nurses play a vital role in protecting, promoting and supporting breastfeeding worldwide. Skilled breastfeeding support from midwives and nurses helps prevent childhood infections and mortality, while boosting cognitive development and decreasing rates of obesity, diabetes and maternal and child cancers. Bonding and attachment are intrinsic to the breastfeeding relationship and foster mental and emotional health and development for both mother and child. Universal breastfeeding could prevent 823,000 child deaths and 20,000 maternal deaths each year and spur significant economic savings.
MCSP Respectful Maternity Care Operational Guidance, Maternal Child Survival Program, 2020
The purpose of this operational guidance is to provide country stakeholders (including policy-makers, program managers and civil society members) with a flexible process to guide the design, implementation, and monitoring of efforts to strengthen RMC and eliminate mistreatment as part of comprehensive MNH programs. This resource is available in English, Spanish, and French.
White Ribbon Alliance Respectful Maternity Care Resources
The White Ribbon Alliance (WRA) has a suite of respectful maternity care resources including RMC guides, policy briefs, reports, and toolkits.
Gender and MNCH: A Review of the Evidence, Bill and Melinda Gates Foundation, 2020
This report provides a landscape and evidence review of how gender influences maternal and newborn health behaviors in low-and middle-income countries. The report draws on existing literature, program reports and evaluations, case studies, and interviews to provide evidence on how gender inequality contributes to challenges for women and their newborns.
Companion of Choice During Labour and Childbirth for Improved Quality of Care, WHO, 2020
This 2020 evidence-to-action brief from WHO and HPR outlines the evidence that continuous support during labour improves childbirth outcomes, including enhancing the physiological process of labour. Research shows that such continuous support shortens labor, increases rates of spontaneous vaginal birth, decreases use of intrapartum analgesia and caesarean section, and increases women’s satisfaction with the childbirth experience. Women supported in this way report less fear and distress during labour, which acts as a buffer against adverse aspects of medical interventions.
Despite the availability of WHO global MDSR and PDSR guidelines and MPDSR policies in many countries, there are many challenges for translating MPDSR policy into implementation at country level. WHO published ‘MPDSR Operational Guidance’, including tools and resources, to support implementation of MPDSR processes in countries.
Maternal and Perinatal Death and Surveillance and Response: Materials to Support Implementation, WHO, 2021
The purpose of the new WHO document “Maternal and Perinatal Death Surveillance and Response (MPDSR): materials to support implementation” is to provide a roadmap for conducting MPDSR in clinical and policy settings. This operational guide has a broad target audience, which may include: clinicians and all participants in clinical care for women and babies, and the maternal and perinatal death review processes as well as public health officials and public health leadership and other stakeholders in maternal and perinatal death reduction, such as planners and managers, in-service trainers, epidemiologists, demographers, policy-makers and professionals working with vital registration systems. This document is a practical step by step guidance, relevant to establish a framework to assess the burden of maternal deaths, stillbirths and neonatal deaths, including trends in numbers and causes of death and on how to link maternal and perinatal death reviews. It is important to generate information about modifiable factors contributing to preventable death, and to use the information to guide action in order to prevent similar deaths in the future. The document promotes confidentiality and a “blame free” culture fostering accountability for results and compelling decision-making.
Maternal Death Surveillance and Response: Technical Guidance, WHO, 2013
This document provides technical guidance on maternal death surveillance and response (MDSR) for healthcare professionals, planners, and managers. MDSR is essential in better understanding maternal death, and ultimately, contributing to the prevention of maternal deaths in the future.
Making Every baby Count: Audit and Review of Stillbirths and Neonatal Deaths, WHO, 2016
This document provides guidance and tools to support the collection of data and information related to stillbirths and neonatal death. Similar to the MDSR approach, this guidance is intended to better understand neonatal deaths and stillbirths to lead the prevention of these deaths in the future, building on systems that are already in place.
The WHO Application of ICD-10 to Deaths During the Perinatal Period: ICD-PM, WHO, 2016
This document presents a standardized system for classifying stillbirths and neonatal deaths. The system also aims to support countries in identifying linkages between neonatal deaths and stillbirths to conditions in pregnant women. The goal is to support the identification of interventions that could present future deaths.
The WHO Application of ICD-10 to Deaths During Pregnancy, Childbirth, and the Puerperium: ICD-MM, WHO, 2012
This document provides guidance to support the collection, analysis, and interpretation of information related to maternal deaths. The document is aimed at supporting healthcare providers, since they are the ones who complete the death certificates, and thus, code the cause of death.