Maternal Mental Health
Global Recommendations and Guidance
This page includes key documents from WHO on maternal mental health, a comprehensive mental health action plan, guidance on community mental health services, a knowledge summary on why maternal mental health matters and what countries can do, as well as a number of tools and guidance to support related programming.
Collaborating for Maternal Mental Wellbeing: Technical Brief on Perinatal Mental Health in Humanitarian Settings, 2023, IAWG Maternal and Newborn Health Sub-Working Group
Mental health and psychosocial support (MHPSS) during the perinatal period is a global issue as the mental health of the mother directly impacts her children. This period is characterized by high risk of common perinatal mental disorders – with one in six pregnant women and one in five postpartum women impacted by a mental health and psychosocial concern during pregnancy or in the first postnatal year. Women in humanitarian settings experience poorer mental health outcomes due to compounded stress and crisis-related factors including nutritional deficiencies, lack of protection and autonomy, GBV, decreased access to family planning services, separation from social support, and lack of access to MHPSS services. These risks have only worsened in the context of COVID-19 as health systems are at or over capacity, with a disproportionate impact on MNH outcomes in LMICs and settings with limited resources.
Objectives include:
- Provide an overview of MHPSS perinatal mental health in emergency response
- Present relevant resources, suggestions for improving collaboration and provision of perinatal mental health
- Share examples of service delivery collaboration
- Culminate with a call to action to progress momentum for perinatal mental health
Comprehensive Mental Health Action Plan, 2013-2030, WHO
This action plan was adopted in 2013 at the sixty-sixth World Health Assembly. In 2019, the plan was extended until 2030. It provides guidance for national action plans and addresses prevention and promotion strategies for all resource settings to promote mental health and well-being for all, prevent mental health conditions for those at-risk, provide care, enhance recovery, promote human rights, and reduce mortality, morbidity and disability for persons with mental disorders.
Objectives include:
- More effective leadership and governance for mental health
- The provision of comprehensive, integrated mental health and social care services in community-based settings
- Implementation of strategies for promotion and prevention
- Strengthened information systems, evidence, and research
Guide for integration of perinatal mental health in maternal and child health services, WHO, 2022
Poor mental health can negatively affect women’s health and the well-being of their babies and families. This guide was written to provide information about how staff in MCH services can provide mental health promotion, prevention, treatment and care. It lists the steps required to plan for integration of perinatal mental health (PMH) care and for assessing its impact. The guide was written primarily for program managers, health service administrators and policy-makers responsible for planning and managing services for women and infants during the perinatal period who wish to integrate mental health care into MCH services or strengthen existing service provision.
Highlights
- Outlines the reason why its important to address PMH care within MNH services, including the consequences of poor mental health, common symptoms, social determinants, risk factors, and protective factors.
- Outlines key elements of quality PMH care (stepped care, supportive environments, promotion, prevention, and treatment).
- Clarifies the steps needed for planning for integration of PMH services.
- Reviews the provision of care for specific populations (for instance adolescents, or those living with HIV or in humanitarian settings – with resources and tools specific to these populations).
- Discusses monitoring and evaluation considerations and examples of indicators.
Guidance on community mental health services: Promoting person-centered and rights-based approaches, WHO, 2021
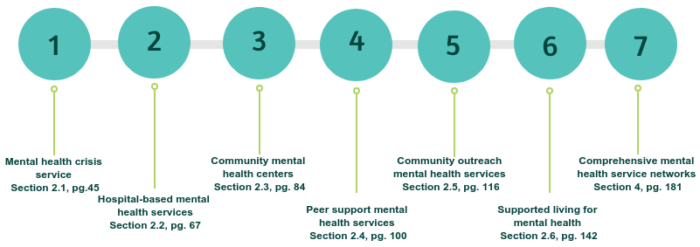
This 2021 comprehensive guidance document includes a detailed description of person-centered and human rights-based approaches in mental health, and examples of good practices worldwide. It provides stakeholders with information and support to develop or transform mental health systems and services to align with international human rights standards. The guidance covers a set of seven technical packages that describe mental health services and guidance for setting up new services:
Key Messages
- People with mental health conditions and psychosocial disabilities face poor quality of care and violations of their human rights, which calls for a change in mental health systems and service delivery.
- Worldwide, examples of good practice, community-based mental health services that are person-centered, recovery-oriented, and adhere to human rights standards exist. In many cases, these show lower costs of service provision than comparable mainstream services.
- Changes in the social sector are required to support access to education, employment, housing, and social benefits for people with mental health conditions and psychosocial disabilities.

Maternal Mental Health: Why it matters and what countries with limited resources can do. PMNCH Knowledge Summary, 2014.
Recognition of maternal mental health has been underprioritized on the health agenda for many low-and middle-income countries (LMICs), despite being fundamental to the psychosocial well-being of women and children. Common perinatal mental disorders (CPMDs) affect the quality of life of both mother and child and have direct and potentially long-term impacts on general well-being and social and economic participation. Maternal mental health conditions, including CPMDs, alcohol use, and psychosis are key causes of pregnancy-related morbidity and mortality. This summary outlines the concept of comprehensive and integrated primary mental health care that considers the interaction of physiological, social, and psychological factors for mental health care provision at the primary and community level as a solution to address maternal mental health.
Key Findings
- Delivery of services to manage mental health conditions at the primary level need to be incorporated into routine antenatal and postnatal care services to reach more women at minimal cost.
- Improvements in maternal and child health outcomes can be achieved through a comprehensive and holistic model of care, including identification of mental health conditions during antenatal and postnatal visits, followed by psychosocial support and appropriate referrals, as needed.
- Improvements in education, employment, and implementation of laws to prevent violence against women are essential to improving maternal mental health.
Additional technical tools and guidance to support countries in the development of mental health policies, plans, and laws to promote improved quality and access include:
- WHO Quality Rights Toolkit, WHO, 2012
- WHO Mental Health Policy and Service Guidance Package, WHO, 2004
- Inter-Agency Standing Committee Guidelines on Mental Health and Psychosocial Support in Emergency Settings, Inter-Agency Standing Committee, 2007

