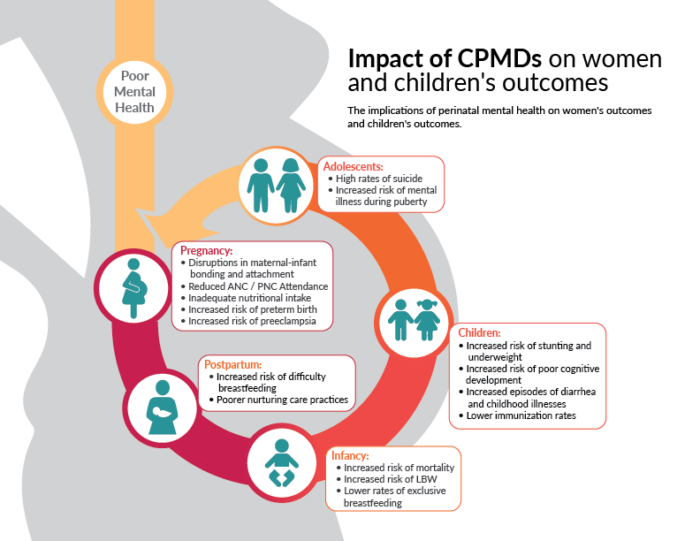
Common perinatal mental disorders (CPMDs), such as depression, anxiety, and somatic disorders, pose significant and lasting implications for women’s health and quality of life, as well as newborn health and development, with intergenerational impacts. [1][2] As highlighted in a recent landscape analysis on maternal mental health, the perinatal period is associated with elevated risk of mental disorders and is a critical time to identify and address mental health concerns.[3] The impact of mental health disorders during the perinatal period deeply affects women, their children, and their families (see graphic below from the landscape analysis on how CPMD affects health outcomes).
Landscape Analysis
The landscape analysis found that risk factors for perinatal mental disorders in low- and middle-income countries (LMICs) range from broader social determinants of health and gender inequality to individual experiences, such as a history of stillbirth or mistreatment by health care providers. Vulnerable groups—adolescents, women experiencing gender-based violence, women living in humanitarian settings, women with a history of obstetric trauma, or those living in poverty—have additional unique perinatal mental health needs.
This analysis also outlines key evidence and gaps related to maternal mental health, promising implementation practices and strategies, and measurement considerations (see this section’s “Key and Emerging Evidence” for more detailed information). Cost-effective and feasible interventions for mental conditions, with demonstrated effectiveness for CPMDs, exist and can be implemented today (see the “Implementation Tools and Resources” section). The merging of maternal, newborn, child, and adolescent health and mental health communities provides a seminal opportunity to accelerate research, learning, and action to address maternal mental health.
NEW WHO world mental health report: Transforming mental health for all
Drawing on the latest evidence, showcasing examples of good practice, and voicing people’s lived experience, WHO’s comprehensive report highlights why and where change is most needed and how it can best be achieved. The report urges all countries to accelerate their implementation of the Comprehensive mental health action plan 2013–2030. It also includes key take-aways from country case studies. While the report addressing the need to transform mental health for all populations, it does specifically address maternal mental health as part of the life course approach (pg. 14), stressing that family building is a risky time for mental health. Maternal mental health is also addressed in the section on supporting caregiver health and well-being (pg. 172), as well as the section on integration of mental health into existing programs and platforms (pg. 219).
This page includes a maternal mental health (MMH) landscape analysis, select sessions from a global MMH technical consultation, a systematic review on Common Perinatal Mental Disorders (CPMDs) in low- and middle-income countries (LMICs), a foundational perinatal mental health series in the Lancet, and a review of the evidence on gender and MNCH that discusses reduction of CPMDs.
This page includes key documents from WHO on maternal mental health, a comprehensive mental health action plan, guidance on community mental health services, a knowledge summary on why maternal mental health matters and what countries can do, as well as a number of tools and guidance to support related programming.
This page includes a mental health action plan to adapt and scale up interventions in low- and middle-income countries (LMICs), a manual for psychosocial management of perinatal depression, a study on implementation technology to scale-up training, a discussion of training grandmothers to deliver evidence-based talk therapy, and select stories and key resources for mental health support for women during the COVID-19 pandemic.
This page includes a video on “Why must maternal mental health be a priority?”, resources on respectful maternal care, and an overview of several organizations committed to:
- Advocating and investing in maternal mental health
- Supporting bereaved parents
- Promoting research on prenatal and postpartum mental health for families, and
- Building communities that put mental health at the core of achieving sustainable growth and development
Citations
[1] World Health Organization. International Statistical Classification of Diseases and Related Health Problems. 11th ed.; 2020. https://icd.who.int/
[2] Galbally M, Snellen M. Providing the evidence for managing depression in pregnancy. Pediatrics. 2020;145(5). doi:10.1542/PEDS.2019-3578
[3] Gelaye B, Rondon MB, Araya R, Williams MA. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. The Lancet Psychiatry. 2016;3(10):973-982. doi:10.1016/S2215-0366(16)30284-X


